64years old male patient presented with unable to speak
This is online E log book to discuss our patient’s de-identified health data shared after taking his/her/guardian’s signed informed consent. Here we discuss our individual patient’s problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs. This e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
I’ve been given this case to solve in an attempt to understand the topic of “patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations, and come up with diagnosis and treatment plan
CHIEF COMPLIANTS :
-Unable to speak since 4 days .Hiccup since 7days
-loose stools, loss of appetite since 3 days
-fever 4 days back
History of presenting illness:
patient is apparently asymptomatic 1and half year back then he developed jaundice for this treatment is given local hospital patient was recoved .1 week back then he developed diarrhoea -5 episodes/day for 1 day which relieved on medical treatment .since 25/12 he is unable to talk.
History of cough present since 10days .
PAST HISTORY :
h/o panic attack one month back secondary to family issues
-DM2 since 6 yrs , on medication ,
-tab Metformin OD , tab Glimiperide OD
-NO HISTORY OF HTN, TB, Asthma, epilepsy, CAD, CVD
Personal History :-
Appetite - lost
Diet - Mixed
Sleep - adequate
Bowel and bladder movements - incontinence
Addictions: Occasional alcoholic ( during functions ) , tobacco chewing daily
Allergies : No allergies
Family history: patient daughter is diagnosed as tb 7years back and treated.
Patient mother is diagnosed as tb 5years back and treated .
GENERAL EXAMINATION :
Patient is conscious ,incoherent , uncooperative
Moderately Built and Moderately Nourished .
Pallor : present
Icterus : absent
Cyanosis: absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
Vitals :-
Temp: Afebrile
BP : 100 / 50 mmHg
PR : 120 bpm
RR : 16 cpm
SPO2 : 98 % at RA
GRBS : 193 mg/dl
SYSTEMIC EXAMINATION:
CNS examination :-
State of consciousness : conscious
Speech : incoherent
Kernigs sign :- negative
Sensory system :-
Pain - Normal
Touch- fine touch - normal
crude touch - normal
Temp - normal
Cranial nerves : intact
CNS :-
Finger nose in coordination - no
Heel knee in coordination - no
CVS : S1 S2 + ,no murmurs ,no thrills
Respiratory System : decreased air entry on left side . Position of trachea - central.
Per abdominal examination:-
Soft , non tender , no signs of organomegaly
Investigations:-
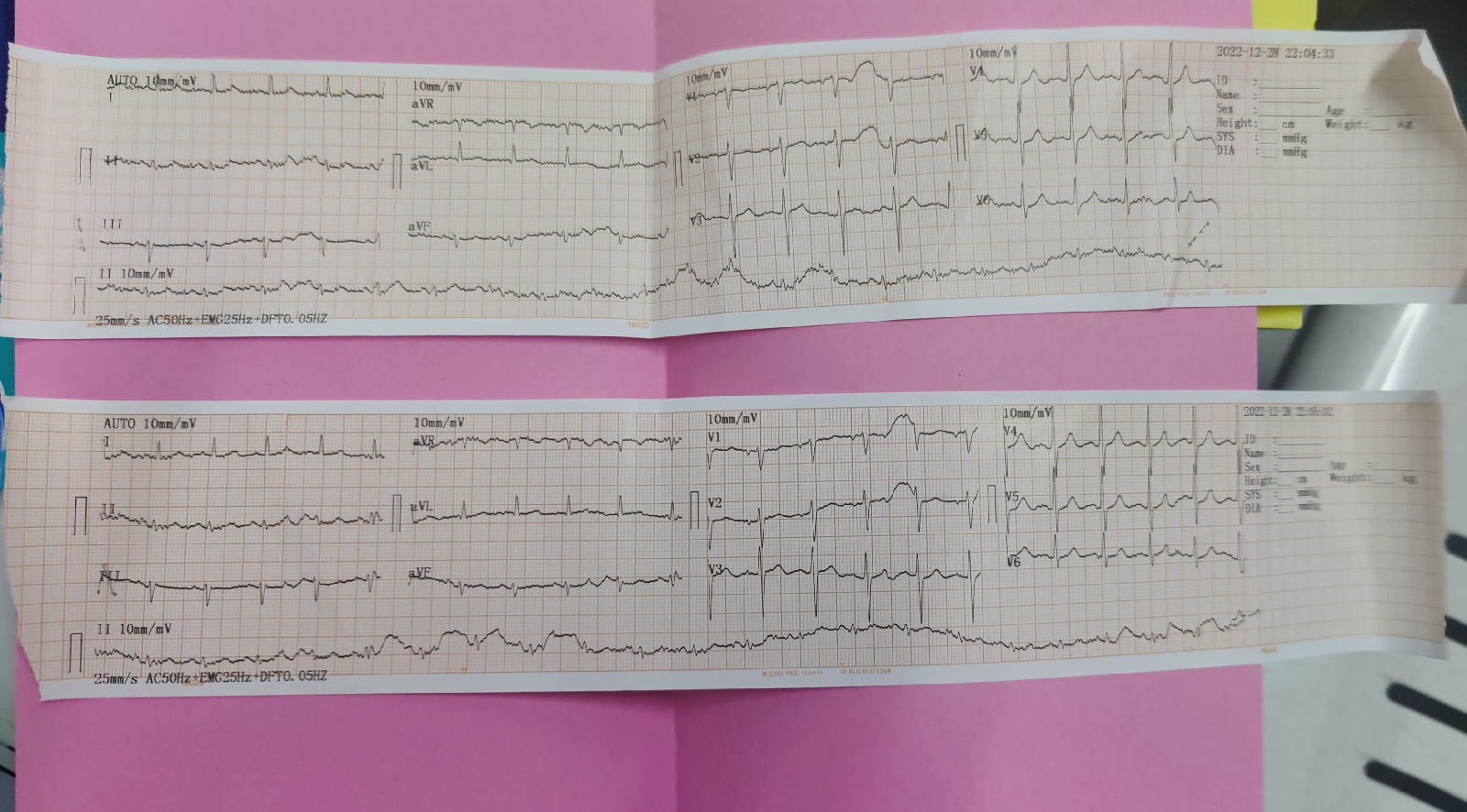
ECG
COMPLETE URINE EXAMINATION
Colour - pale yellow
Appearance - clear
Reaction - acidic
Specific gravity - 1.010
Albumin -nil
Sugar -nil
Bile salts - nil
Bile pigments- nil
Pus cells - 2-3cells(normal 0-5/HPF)
Epithelial cells- 2-3 cells(normal 0-5HPF)
RBC -nil (normal 0-5/HPF)
Crystals-nil
Casts-nil
Amorphous deposits-absent
BLOOD UREA -124mg/dl(normal 17-50mg/dl)
APTT
APTT TEST- 31sec(normal 24- 33sec)
Bleeding and clotting time
Bleeding time- 2min 30sec(normal2 -7 min)
Clotting time- 5min (normal 1- 9min)
PROTHROMBIN TIME - 15sec ( normal 10 -16 sec)
DIAGNOSIS :
Altered sensorium secondary to
meningoencephalitis
Management:-
1) IVF 0.9 %NS IV @ 50 ml / hr
2) Inj , 1 amp Optineuron in 500 ml NS IV /OD
3) tab Ecosprin AV 75/10 RT / OD / HS
4) GRBS monitoring 6 th hrly
5) Inj Thiamine 200 mg IV/BD in 100 ml NS
29/12/2022 at 12 pm
on 30/12/2022
icu
bed 6
day 2
unit 3
dr.nikitha (sr )
dr.vamshi krishna ( pg 3 )
dr. nishitha ( pg 2 )
dr.govardhini reddy ( pg 1 )
dr. meghana ( intern )
dr. tejarshini ( intern)
s:
no fever spikes
stools passed
o :
patient is drowsy but arousable
bp :120/80 mm hg
pr :- 102 bpm
rr : 17 cpm
temp : 98 f
spo2 : 98 % at ra
grbs :- 275 mg/dl
i/o : 1500/900 ml
cns :- gcs : e3v4m6
cvs : s1 , s2 heard, no murmurs
rs : bae + , decreased air entry on left side , crepts +
p/a:- soft , non tender
a :-
- altered sensorium secondary to meningoencephalitis (? tb )
- left sided pneumonia ( ?tb )
p :
1) ivf 0.9 %ns iv @ 75 ml / hr
2) nebulization with duolin - 8th hrly , budecort - 12 th hrly
3) inj , 1 amp optineuron in 500 ml ns iv /od
4) inj .thiamine 200 mg iv/bd in 100 ml ns
5) inj .monocef 2 gm iv/bd
6) inj . clindamycin 600 mg iv / tid
7) inj . dexa 6 mg iv / tid
8) t.baclofen 10 mg rt/tid
9) att therapy
10) grbs monitoring 6 th hrly
11) vitals monitoring 6 th hrly
12) temp monitoring 4 th hrly
13) inj h. actrapid insulin sc
31/12/2022:
Bed 6
Day 3
Unit 3
Dr.Nikitha (SR )
Dr.Vamshi Krishna ( PG 3 )
Dr. Nishitha ( PG 2 )
Dr.Govardhini Reddy ( PG 1 )
Dr. Meghana ( intern )
Dr. Tejarshini ( intern)
S :
Pt in altered sensorium
O :
Patient is drowsy but arousable
BP :120/80 mm hg
PR :- 102 bpm
RR : 17 cpm
Temp : 98 F
Spo2 : 98 % at RA
GRBS :- 246 mg/dl
I/O : 2100/1100 ml
CNS :- GCS : E2V1M4
Right. Left
Tone :- UL hypo hypo
LL hypo hypo
Power :- UL : moving all four limbs in LL : response to pain
CVS : S1 , S2 heard, no murmurs
RS : BAE + , decreased air entry on left side , crepts +
P/A:- soft , non tender
A :-
- Altered sensorium secondary to meningoencephalitis (? TB )
- Left sided pneumonia ( ?TB )
P :
1) IVF 0.9 %NS IV @ 75 ml / hr
2) Nebulization with duolin - 8th hrly , budecort - 12 th hrly
3) Inj , 1 amp Optineuron in 500 ml NS IV /OD
4) Inj .Thiamine 200 mg IV/BD in 100 ml NS
5) Inj .Monocef 2 gm IV/BD
6) Inj . Clindamycin 600 mg IV / TID
7) Inj . Dexa 6 mg IV / TID
8) T.Baclofen 10 mg RT/TID
9) ATT therapy
10) GRBS monitoring 6 th hrly
11) vitals monitoring 6 th hrly
12) Temp monitoring 4 th hrly
13) Inj H. Actrapid insulin SC TID acc to GRBS












Comments
Post a Comment