1801006024-LONG CASE
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
13 Years old female student by occupation came to casuality with
CHIEF COMPLAINTS:
Shortness of breath since 2 days (decreased now)
4 episodes of vomitings since 2days 10pm
HISTORY OF PRESENTING ILLNESS :
Patient was apparently asymptotic till the age of 11years
She was sent to hostel for studies
After few days of hostel stay she noticed that she has bilateral neck swellings
So she was taken to RMP with complaints of neck swellings,fever and cough on and off
RMP has initiated her on ATT as her mother has also has Tb
They used ATT for 2months started in 2021 june
After initiating ATT fever increased so they stopped ATT and was referred to Hyd by the RMP
Patient was taken to hospital where she was evaluated for kochs but none of the investigations showed AFB,at that time she also had complaints of knee pains and wrist joint pains
In view of joint pains she was referred to x hospital
In X hospital they suspected it to be autoimmune and started her on Tab Wysolone and Tab HCQ ,which she used for 15 days and stopped and later did not go there for follow up
She was taken to another local hospital with c/o joint pains,facial puffiness,pedal edema,fever ,cough
Lymph node biopsy was done in May 2022 ?reactive(no report available but attendor was informed that it was negative for kochs)
So Mycobacterial gene expert test was done on blood sample which was also negative
But she was initiated on ATT empirically on may/2022.
10-15days before starting ATT attendors have noticed that she is developing facial rash and Hair loss,due to hair loss scalp rash also became evident.
PAST HISTORY :
Known case of tb (1year back used att for 6 months)
N/k/c/o hypertension, DM, epilepsy, Asthma
BIRTH HISTORY:
1st child
2nd degree consanguineous marriage
Born in 2010
LSCS - delivery
Father has no idea about immunisation status
FAMILY HISTORY :
2014 mother diagnosed with TB-expired in 2022 sept(did not use ATT regularly)
PERSONAL HISTORY:
Diet - Mixed
Appetite - Decreased appetite
Decreased urineoutput
Sleep - adequate
Addictions - None
TREATMENT HISTORY :
Used Anti Tubercular therapy for 6 months for extra pulmonary tb.
GENERAL EXAMINATION :
The patient is conscious, coherent, cooperative, and well oriented to time, place and person.
Moderately built and Moderately nurished
Pallor is present
Edema of Lower Limbs is present
No icterus, cyanosis, clubbing, lymphadenopathy
VITALS:
,Temp: 98.4 F
PR: 126 bpm
BP: 130/90 mm Hg
RR: 26 cpm
SPO2: 98%
SYSTEMIC EXAMINATION :
Patient is examined in a well lit room and in a sitting position
RESPIRATORY SYSTEM:
Bilateral Air entry present
Vocal resonance is decreased in affected area
Dull note on percussion in affected region
C V S :
S1,S2 heard
Pericardial rub
No murmur
PER ABDOMINAL EXAMINATION:
INSPECTION: Shape of Abdomen - mild distended, No sinuses, fistulas. Umbillicus - Central, not everted
PALPATION: Inspectory Findings Confirmed
Soft, Tenderness present in right and left hypochondrium
Epigastrium
PERCUSSION : Shifting dullness
AUSCULTATION: Bowel sounds Heard
C N S :
No focal neurological deficits
HIGHER MENTAL FUNCTIONS-
Normal
Memory intact
CRANIAL NERVES :Normal
SENSORY EXAMINATION :
Normal sensations felt in all dermatomes
MOTOR EXAMINATION :
Normal tone in upper and lower limb
Normal power in upper and lower limb
Normal gait
REFLEXES:
Normal reflexes elicited- biceps, triceps, knee and ankle reflexes elicited
CEREBELLAR FUNCTION :
Normal function
No meningeal signs were elicited
INVESTIGATIONS :
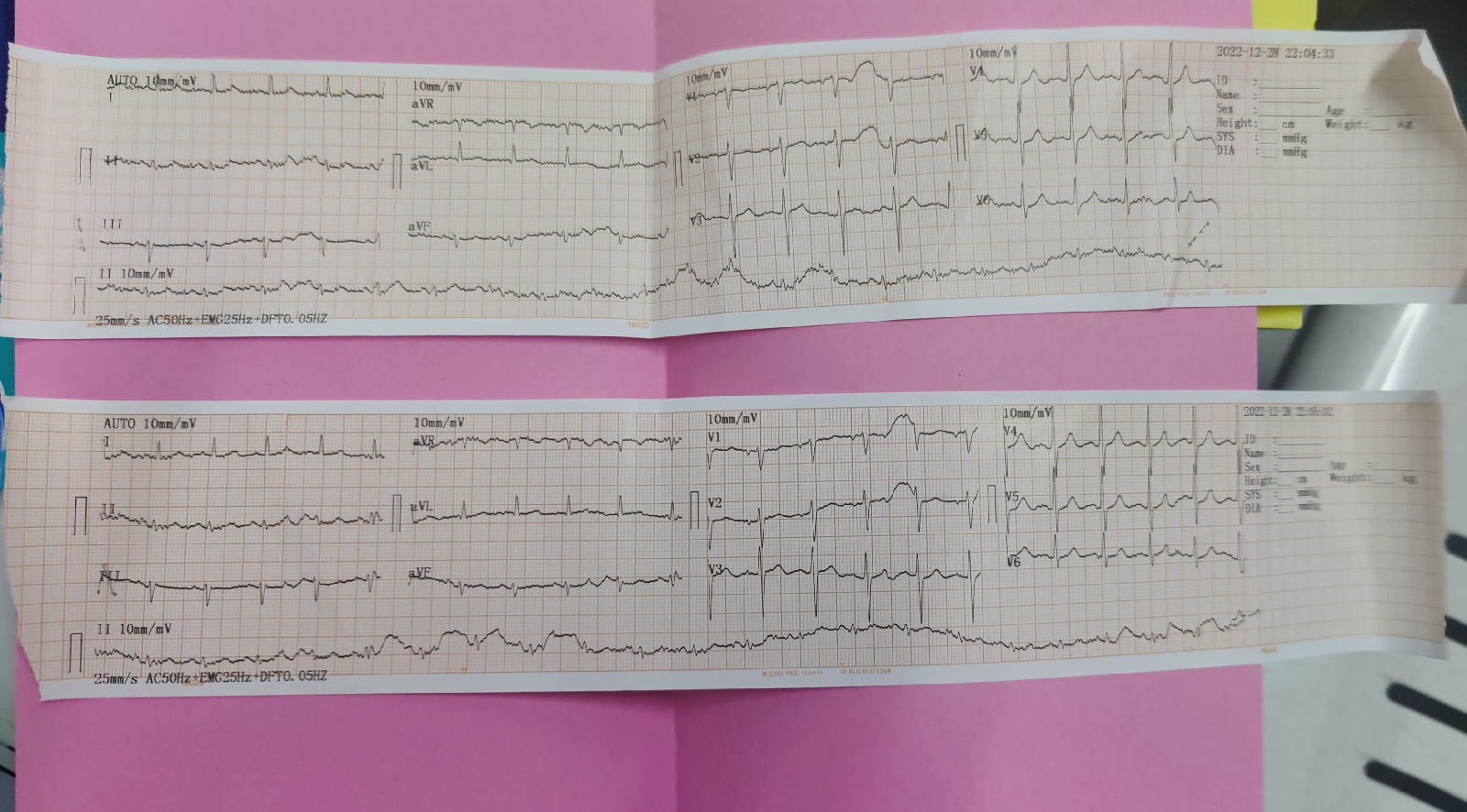
ECG -
Hemogram :
HB -6.8 gm/dlPeripheral smear - Anisopoikilocytosis with macrocytes ,tear drop ,microcytes
Other investigation:
On spot urine protein -10gm/dl
Findings -
Clinical images
DIAGNOSIS :
?Autoimmune disease ? Glomerulonephritis secondary to ? Lupus
TREATMENT :
1. FLUID RESTRICTION LESS THAN 1.5L/DAY
2. SALT RESTRICTION LESS THAN 1.2GM/DAY
3. INJ. LASIX 40 MG IV/BD
4. INJ. METHYLPREDNISOLONE 250 MG IN 100ML NS IV/OD
5. TAB. ALDACTONE 25MG PO/OD
6. TAB. SHELCAL 500 MG PO/OD
7 VITALS MONITORING



























Comments
Post a Comment