1801006024 - SHORT CASE
1801006024 - SHORT CASE
This is an online E logbook to discuss our patients' de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from the available global online community of experts intending to solve those patients' clinical problems with the collective current best evidence-based inputs. This e-log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box are welcome.
I have been given this case to solve in an attempt to understand the topic of " Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, and investigations, and come up with a diagnosis and treatment plan.
CHIEF COMPLAINTS:
Generalised weakness since 16 days
Shortness of breath since 16 days
Easy fatigability since 16 days
HISTORY OF PRESENTING ILLNESS:
patient was apparently asymptomatic 16 days back he developed generalised weakness insidious in onset, gradually progressive
Shortness of breath of grade 2
Easy fatigability present
No c/o fever, nausea, vomiting, chest pain, pain abdomen, blood in stools, loose stools, sweating
1 year back, then he developed jaundice and generalised weakness for which he took herbal medicines for 10 days and was resolved.
PAST HISTORY:
Not a k/c/o DM/HTN/TB/ Epilepsy/CVA/CAD/Asthma
PERSONAL HISTORY:
decreased appetite since 5-6 months
Takes vegetarian diet
Bowels and bladder habits are regular
Disturbed sleep
Occassional alcohol drinker stopped 1 year back
FAMILY HISTORY:
No significant family history
TREATMENT HISTORY:
No significant history
GENERAL EXAMINATION:
patient is conscious,cohorrent cooperative
Pallor and icterus is present
No signs of cyanosis, clubbing, lymphadenopathy, pedal edema
Vitals:
Temp: afebrile
PR: 106 bpm
RR: 20 /min
BP: 130/90 mm hg
Systemic examination:
CVS: S1 S2 heard, No Murmur
RS: Bilateral air entry present
CNS: No focal neurological deficit
Per Abdomen : soft, non tender, no organomegaly
Bowel sounds heard
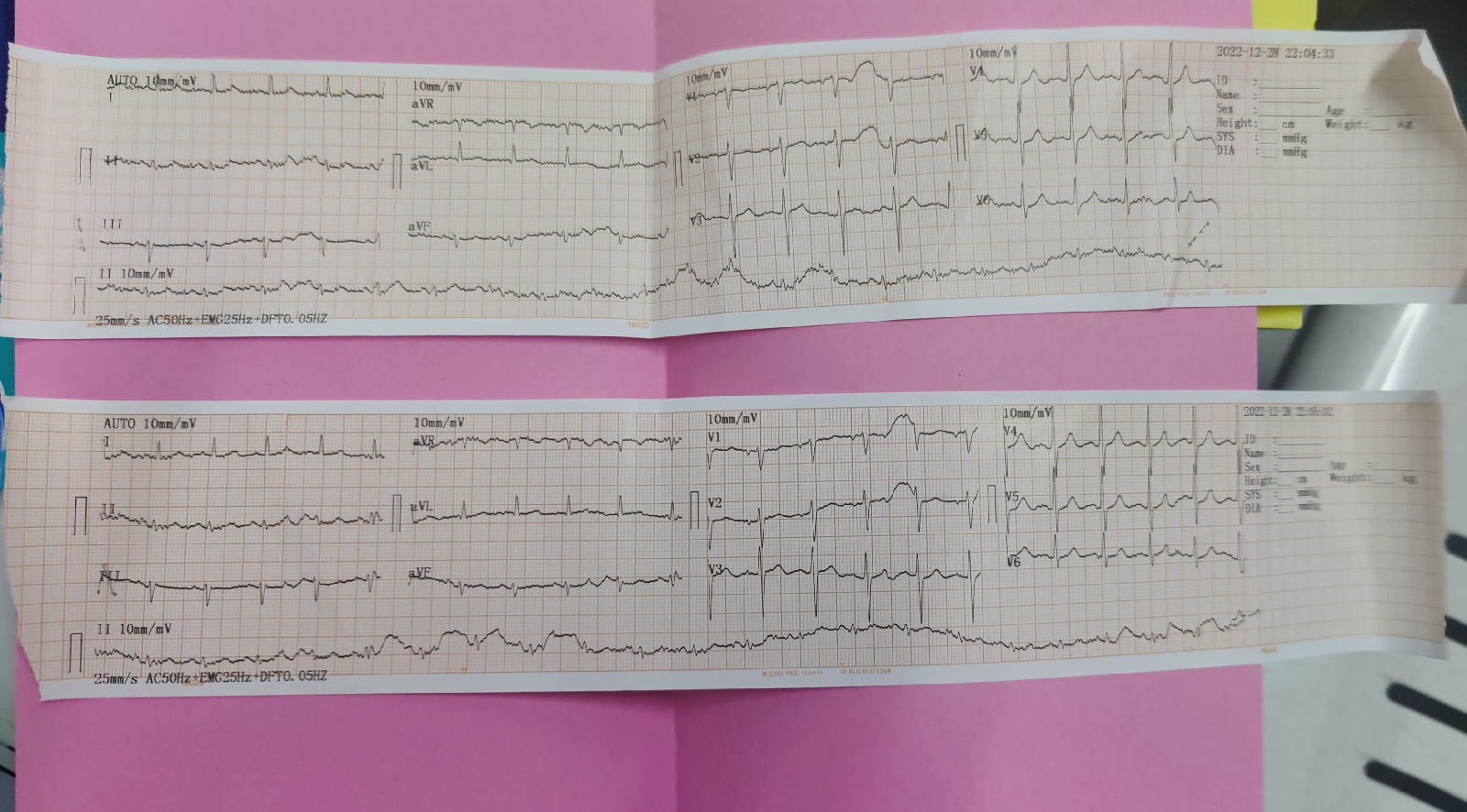
INVESTIGATIONS :
CHEST X RAY :
Diagnosis: Anemia secondary to vit b12 deficiency iron deficiency (dimorphic anemia)
Treatment:
Inj. VITCOFOL 1000mg/IM/OD
Dermatology opinion was taken on 9/3/23 i/v/o hyperpigmented scaly lesions over abdomen, groin, inner thighs, buttocks and legs
On 10/3/23
27 year old male came with c/o generalised weakness and shortness of breath since 10 days
S
1 fever spike
O
Pt is c/c/c
BP-130/70 mmhg
PR- 92bpm
Temp- 98.5F
CVS- S1,S2 heard, no murmurs
RS- B/L Air entry present
P/A: soft, non-tender
CNS: HMF intact, NFND
A
Anemia Secondary to B-12 deficiency and Iron deficiency (Dimorphic) with Tinea Corporis ET Cruris +Statis Dermatitis
P:
Inj. VITCOFOL 1000mg/IM/OD
LULIFIN CREAM L/A BD
LIQUID PARAFFIN L/A BD
TAB. TECZINE 5mg
Follow up on phone call -
Normal appetite
Recent lab report done on 14th In Nalgonda
Hemoglobin:7.6gm/dl
Using medication -
Inj. VITCOFOL 1000mg/IM/OD
LULIFIN CREAM L/A BD
LIQUID PARAFFIN L/A BD
TAB. TECZINE 5mg SOS




















Comments
Post a Comment