35 years old female patient came to casuality
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
35 YEARS OLD FEMALE PATIENT CAME TO CASUALITY WITH
Chief complaints :
Chest pain since 6months
Shortness of breath since 5 months
History of presenting illness :
Patient was apparently asymptomatic 6months back then she developed chest pain (both right and left side) which is insidious in onset gradually progressive in nature associated with chest tightness. Chest pain and tightness are more after eating food associated with excessive sweating. Then she developed shortness of breath which is insidious onset gradually progressive (grade2 to grade3) .
Orthopnea - present at rest
No H/o paraoxysomal nocturnal dyspnea
No H/o giddiness ,pedal edema , cough, cold ,pain in abdomen ,vomiting
Past history: Not a k/c/o DM,TB , epilepsy,HTN ,asthma
Personal history:
Married
Appetite: normal
Bowel and bladder: regular
Addictions : no
Sleep: adequate
Family history: No significant family history
Treatment history: No significant treatment history
General examination :
Patient is conscious ,coherent ,cooperative
Moderately Built and Moderately Nourished
Pallor : absent
Icterus : absent
Cyanosis: absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
Vitals :-
Temp: Afebrile
BP : 140 / 80mmHg
PR : 73 bpm
RR : 22cpm
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection: chest shape normal,
No scars , no engorged veins
Movement of chest both sides
AUSCULTATION :
Bilateral air entry
Normal vesicular breath sounds
PALPATION:
Trachea central
Cvs :
S1,S2 - heard
No murmur
Abdominal examination:
Shape : scaphoid
Tenderness -no
Free fluid -no
Liver,spleen -not palpable
CNS:
Higher mental status intact
Reflexs are intact
No focal neurological deficit
INVESTIGATIONS:
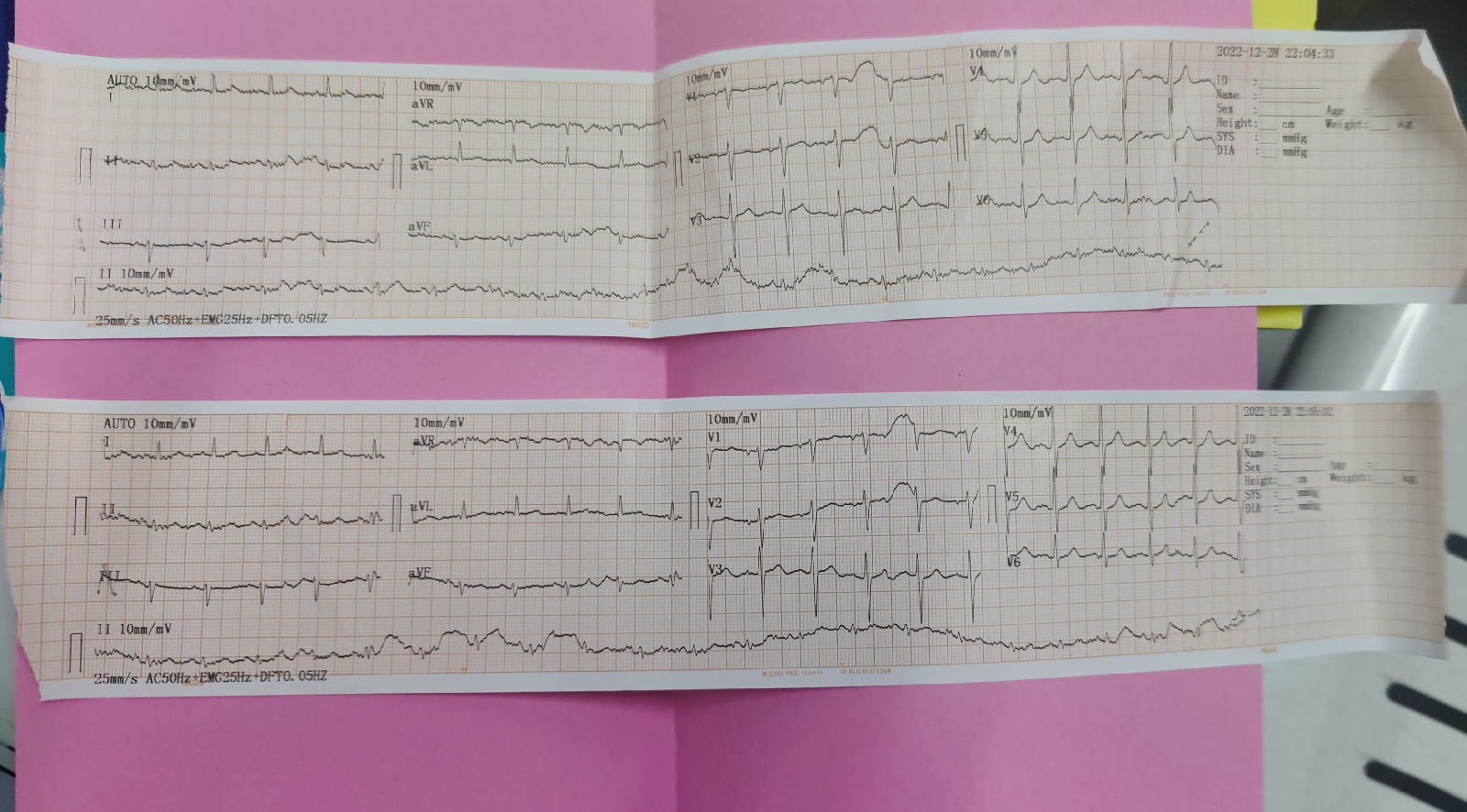
ECG :
Chest x ray PA view :
USG :
RFT :
Hemogram:
CUE :
LFT :
Diagnosis : dyspnea under evaluation








Comments
Post a Comment