45 YEARS OLD MALE PATIENT CAME TO CASUALITY
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan. is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
45 YEARS OLD MALE PATIENT CAME TO CASUALTY WITH
CHIEF COMPLIANTS :
Giddiness since 4hrs
Shivering since 1hr
Vomiting 1 episode
History of presenting illness:
Patient was apparently asymptomatic 4hours back then he developed giddiness,sudden in onset , immediately after waking up from the sleep (rotational effect ).No history of tinnitus/ ringing sensation
Shivering since 1 hour . vomiting 1 episode,non bilious ,watery ,non projectile ,not blood stained .
No history of fever ,cough ,SOB,loose stools,Pain abdomen .
Past history :
N/K/c/o HTN ,DM ,TB ,Asthma , Epilepsy
Personal history:
Diet - mixed
Appetite -Normal
Bowel and bladder - regular
Sleep - adequate
Addiction - Alcohol intake since 20years
3 quarters per day
Treatment history :
No significant treatment history
Family history: Not significant
General examination :
Patient is conscious ,coherent ,cooperative
Moderately Built and Moderately Nourished
Pallor : absent
Icterus : present
Cyanosis: absent
Clubbing : absent
Lymphadenopathy : absent
Edema : absent
Vitals :-
Temp: 96.8F
BP : 130 / 80mmHg
PR : 90 bpm
RR : 18cpm
SYSTEMIC EXAMINATION:
Respiratory system:
Inspection: chest shape normal,
No scars , no engorged veins
Movement of chest both sides
AUSCULTATION :
Bilateral air entry
Normal vesicular breath sounds
PALPATION:
Trachea central
Cvs :
S1,S2 - heard
No murmur
Abdominal examination:
Shape : scaphoid
Tenderness -no
Free fluid -no
Liver,spleen -not palpable
CNS:
Gait - Ataxic gait
HIGHER MENTAL FUNCTIONS:
Conscious, oriented to time place and person.
Speech : Normal
Behavior : is not aggitated and not irritable
Memory : Normal
Intelligence : Normal
CRANIAL NERVE EXAMINATION:
1st : Normal
2nd : visual acuity is normal
3rd,4th,6th : Normal
5th : sensory intact
7th : Ability to blow cheeks
8th : No abnormality noted.
9th,10th : palatal movements present and equal.
11th,12th : normal.
MOTOR EXAMINATION: Right Left
RT LT
POWER - UL 5/5. 5/5
LL 5/5. 5/5
TONE. - U L N N
LL N. N
REFLEXS - Rt. Lt
biceps. 3+ 3+
Triceps 3+. 3+
Supinator. 1+ 2+
Knee 3+ 3+
Ankle 2+ 2+
Plantar B /L flexed
SENSORY EXAMINATION:
SPINOTHALAMIC SENSATION:
Crude touch - normal
pain felt on upper limb
Supraorbital pressure felt
Sternal rub pain felt
DORSAL COLUMN SENSATION:
Fine touch able to perceive on right upper and lower limb
CEREBELLAR EXAMINATION:
Finger nose test able to perform with both hand
Nystagmus seen
SIGNS OF MENINGEAL IRRITATION: absent
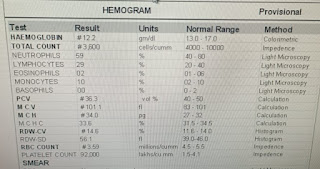
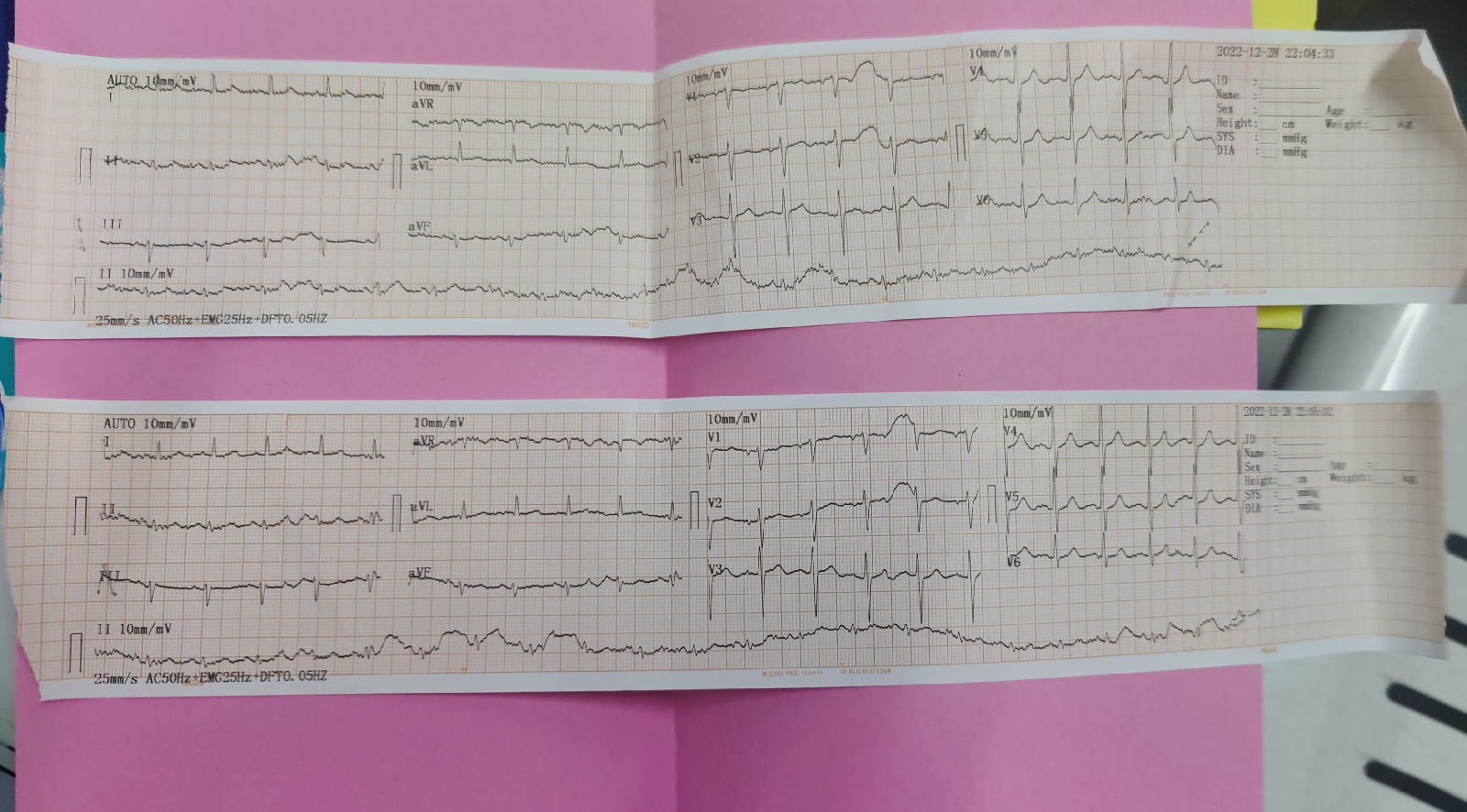
INVESTIGATIONS :
Diagnosis:
? Alcoholic liver disease
? Alcoholic gastritis
? WERNICKES ENCEPHALOPATHY
Clinical images :






Comments
Post a Comment